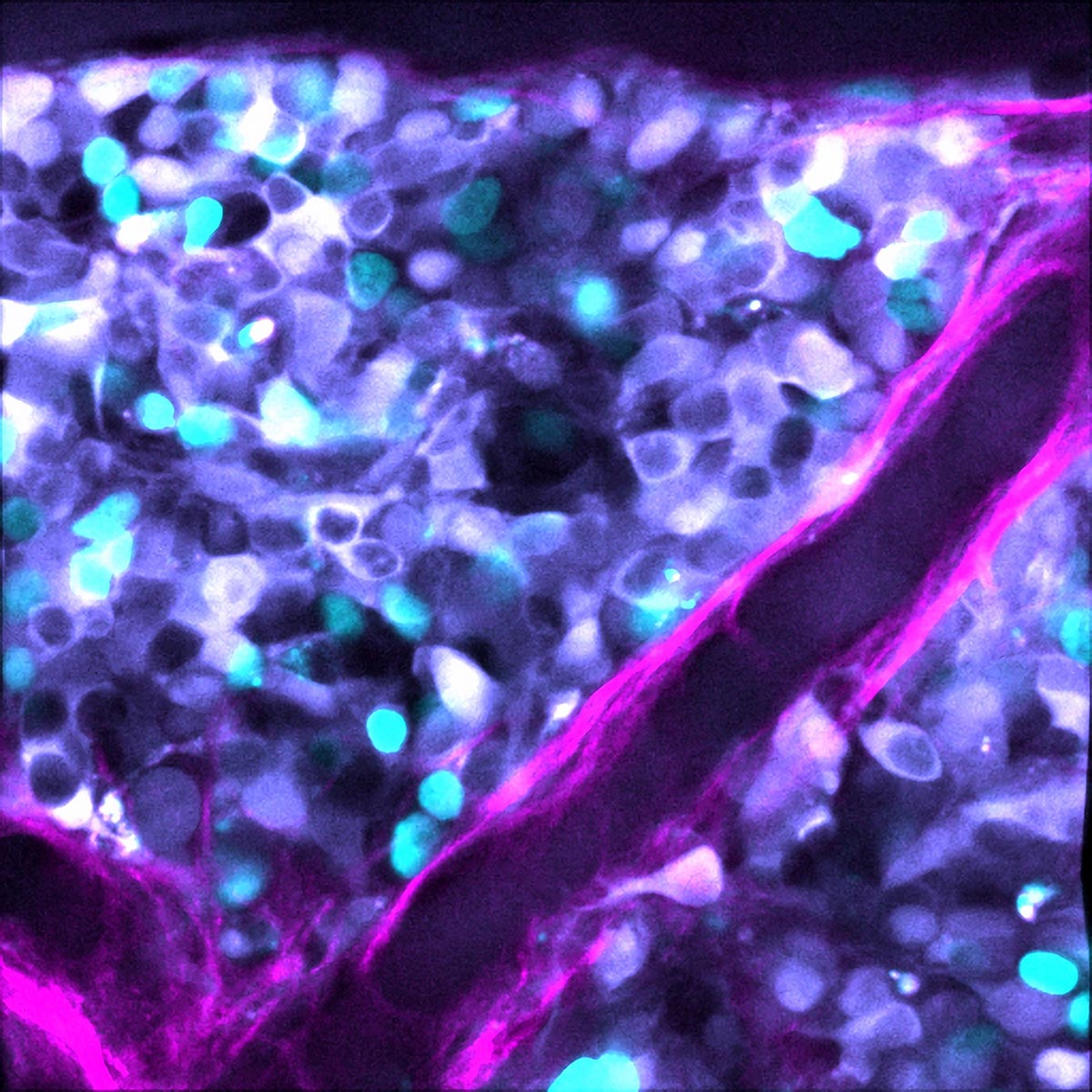

Neuroblastoma cells (cyan) increasing as a tumor and the surrounding collagen matrix (magenta). The cells are expressing a biosensor (JNK-KTR) that reads out one-cell JNK activity in response to chemotherapy therapy. Credit: Max Nobis / Garvan
Inherent ‘noise’ in the system of gene expression in tumor mobile dying, is an additional tool cancer cells use to resist chemotherapy procedure.
Most cancers cells have an innate randomness in their capacity to respond to chemotherapy, which is a different resource in their arsenal of resisting treatment method, new exploration led by the Garvan Institute of Health care Analysis demonstrates.
Being familiar with why some tumor cells turn out to be resistant to chemotherapy is a main problem in most cancers investigation, as chemotherapy is continue to a frontline cure for most cancers.
The new exploration reveals that tumor cells from neuroblastoma – cancer that develops in the body’s ‘fight or flight’ sympathetic nervous procedure – can transfer concerning states of responding, or not, to chemotherapy.
“We showed there is ‘noise’ in the process of mobile dying, which is what comes about to most cancers cells with chemotherapy procedure – and that this inherent sounds, or randomness, in the system of gene expression is an vital factor of chemoresistance,” suggests Affiliate Professor David Croucher, Head of the Network Biology Lab at Garvan.
About 15{35112b74ca1a6bc4decb6697edde3f9edcc1b44915f2ccb9995df8df6b4364bc} of folks with neuroblastoma never answer to chemotherapy procedure.

Neuroblastoma cells (cyan) expanding as a tumor and the surrounding collagen matrix (magenta). The cells are expressing a biosensor (JNK-KTR) that reads out one-cell JNK exercise in response to chemotherapy treatment. Credit: Max Nobis / Garvan
“Our results propose that genetics do not account for every little thing other levels of regulation and other mechanisms of tumor development can also underpin drug response, so we require to take into consideration them,” states Dr. Sharissa Latham, co-direct creator on the analyze.
The group showed that after neuroblastoma cells reach a point out of resisting chemotherapy, they can not go again, suggesting there is a compact window in which treatment could operate on a tumor cell before it is locked in.
“Combining chemotherapy with prescription drugs that goal this noise within just tumors may well have the ideal final results as a initial-line treatment method after analysis, before tumors lock into a point out of resistance,” claims Associate Professor Croucher. This flips on its head the typical protocol for clinical trials in cancer where by a new procedure is supplied to people who have fatigued all other treatment method solutions.
The new study is revealed in the journal,
Neuroblastoma cells (cyan) growing as a tumor and the surrounding collagen matrix (magenta). The cells are expressing a biosensor (JNK-KTR) that reads out single-cell JNK activity in response to chemotherapy treatment. Credit: Max Nobis / Garvan
Noise in the tumor system
The researchers used mathematical modeling to narrow down the ‘noise’ signals in the pathways of cell death in neuroblastoma tumors. They then applied that to patient cell samples, using cutting-edge imaging to look at single cells, en masse, to visually isolate the cells that didn’t respond to treatment.
The found a marker for resistance – a set of proteins involved in the process of cell death, known as apoptosis.
“We wanted to figure out what underlies that randomness. What is it about those cells and can anything be manipulated to make them respond,” says Dr. Latham.
The team identified certain classes of approved drugs that might be combined with chemotherapy to stabilize expression of the genes involved in cell death, or by changing the innate threshold that may tip a tumor cell into a resistant state.
The next step is to start progressing the work to clinical trial.
Reference: “Memory of stochastic single-cell apoptotic signaling promotes chemoresistance in neuroblastoma” 3 March 2023, Science Advances.
DOI: 10.1126/sciadv.abp8314
This research was supported by Cancer Institute NSW, NHMRC, Cancer Council NSW, NBCF and the Medical Research Future Fund.
Associate Professor David Croucher is a Conjoint Professor at St Vincent’s Clinical School, Faculty of Medicine and Health, UNSW Sydney. Dr. Sharissa Latham is a Conjoint Lecturer at St Vincent’s Clinical School, Faculty of Medicine and Health, UNSW Sydney.









