Vital Takeaways
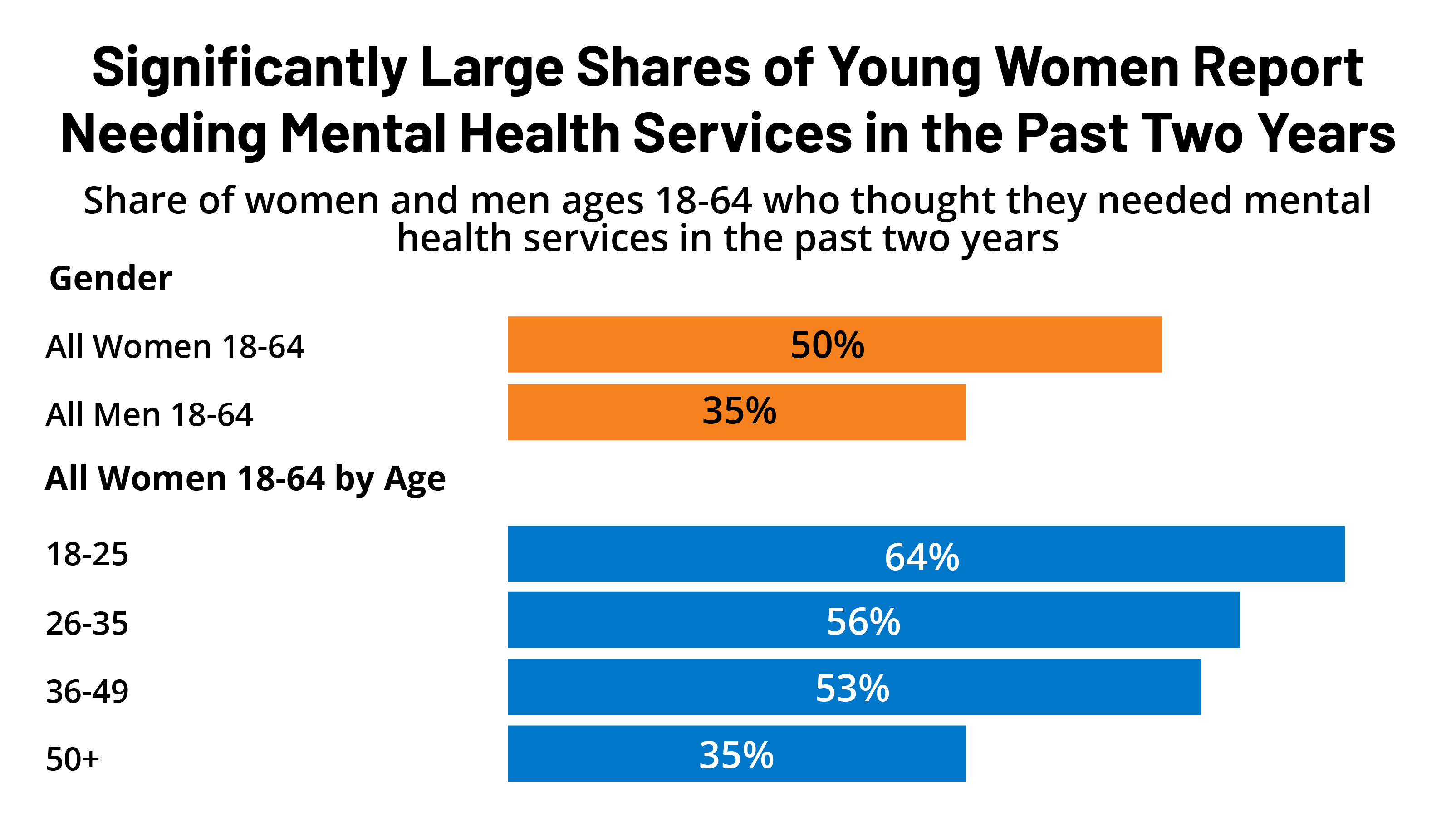
- A noticeably bigger share of women (50{35112b74ca1a6bc4decb6697edde3f9edcc1b44915f2ccb9995df8df6b4364bc}) than guys (35{35112b74ca1a6bc4decb6697edde3f9edcc1b44915f2ccb9995df8df6b4364bc}) thought they required psychological wellness providers in the past two decades. Amid those who considered they essential mental wellbeing care, about six in ten women of all ages and guys sought treatment in the previous two yrs.
- Just about two-thirds of youthful gals ages 18-25 report needing mental wellbeing care in the earlier two decades in comparison to one-3rd of women of all ages ages 50-64.
- Among the all ladies ages 18-64 who believed they desired mental wellness services in the past two a long time, just half attempted and had been ready to get an appointment for psychological wellbeing treatment, 10{35112b74ca1a6bc4decb6697edde3f9edcc1b44915f2ccb9995df8df6b4364bc} tried out but were being not able to get an appointment, and 40{35112b74ca1a6bc4decb6697edde3f9edcc1b44915f2ccb9995df8df6b4364bc} did not request treatment.
- Nearly 50 percent of girls who wanted mental overall health products and services and tried using to get care were being ready to get an appointment inside of a thirty day period, but more than just one-third of females experienced to wait around much more than a thirty day period. Among individuals who could not get an appointment, ladies cite limited supplier availability and cost as the key explanations they have been unable to obtain mental well being care.
- Two in 10 privately insured females with a mental overall health appointment in the earlier two many years say their service provider did not acknowledge their insurance.
- Sixty percent of gals had a telemedicine/telehealth go to in the past two a long time. Psychological well being care was the third most typical purpose girls cited for accessing telehealth/telemedicine providers, with 17{35112b74ca1a6bc4decb6697edde3f9edcc1b44915f2ccb9995df8df6b4364bc} declaring it was the key intent of their most current telemedicine pay a visit to. The vast majority report that the excellent of their telehealth stop by was the exact same as an in-human being check out.
Introduction
Psychological overall health has emerged as a swiftly developing concern in recent years, with 90{35112b74ca1a6bc4decb6697edde3f9edcc1b44915f2ccb9995df8df6b4364bc} of Americans indicating there is a mental well being disaster in a modern KFF-CNN poll. Girls knowledge various psychological health circumstances a lot more usually than adult men, and some also expertise psychological well being problems that are special to girls, these as perinatal despair and premenstrual dysphoric ailments that may well come about when hormone degrees alter. Info from the National Middle for Health and fitness Stats present that across all age groups, ladies were almost 2 times as possible to have despair and stress than adult males. The COVID-19 pandemic, the opioid epidemic, and racism are amongst frequently cited stressors that have exacerbated extensive-standing psychological health challenges and prompted developing demand from customers for psychological health and fitness providers in the previous two a long time, specifically among females.
This temporary delivers new facts from the 2022 KFF Women’s Health Study (WHS), a nationally representative survey of 5,145 women and 1,225 gentlemen ages 18-64 conducted mostly on line from May well 10, 2022, to June 7, 2022. In addition to several subject areas similar to reproductive health and perfectly-becoming, the survey questioned respondents about their experiences accessing mental well being providers in the previous two many years. This concern temporary offers KFF WHS data on mental wellbeing providers obtain between self-discovered women and guys ages 18-64, and it also normally takes a closer seem at mental overall health protection among the gals. People today of all genders, which include non-binary people today, had been requested these thoughts on the other hand, there are insufficient data to report on non-cisgendered men and women. See the Methodology section for aspects.
Utilization of Mental Wellness Products and services
Gender Distinctions
Fifty percent of gals ages 18-64 (50{35112b74ca1a6bc4decb6697edde3f9edcc1b44915f2ccb9995df8df6b4364bc}) assumed they needed psychological overall health services in the past two decades (Determine 1) and a considerably lesser share of males report they essential mental wellbeing care (35{35112b74ca1a6bc4decb6697edde3f9edcc1b44915f2ccb9995df8df6b4364bc}). Research have prolonged documented gender disparities in the premiums and forms of psychological wellness ailments. Amid those who imagined they essential care, nonetheless, identical fees of females and gentlemen report trying to get care. Sixty p.c of gals tried to make an appointment for psychological well being compared to 56{35112b74ca1a6bc4decb6697edde3f9edcc1b44915f2ccb9995df8df6b4364bc} of adult men.
Will need and Care Trying to get
Approximately two thirds (64{35112b74ca1a6bc4decb6697edde3f9edcc1b44915f2ccb9995df8df6b4364bc}) of gals ages 18-25 believed they needed psychological health and fitness products and services at some issue in the previous two many years in comparison to just 35{35112b74ca1a6bc4decb6697edde3f9edcc1b44915f2ccb9995df8df6b4364bc} of girls ages 50-64 (Determine 2). Previous results from the 2020 KFF WHS revealed that far more than half of females (51{35112b74ca1a6bc4decb6697edde3f9edcc1b44915f2ccb9995df8df6b4364bc}) mentioned that worry or pressure linked to the coronavirus had affected their psychological health. Other studies clearly show that younger grownups, especially gals, knowledgeable large incidence of depression and loneliness in the course of the early levels of the pandemic.
Extra than half of gals with low incomes (< 200{35112b74ca1a6bc4decb6697edde3f9edcc1b44915f2ccb9995df8df6b4364bc} of the federal poverty level (FPL)) (55{35112b74ca1a6bc4decb6697edde3f9edcc1b44915f2ccb9995df8df6b4364bc}) and women with Medicaid coverage (58{35112b74ca1a6bc4decb6697edde3f9edcc1b44915f2ccb9995df8df6b4364bc}) thought they needed mental health care in the past two years compared to less than half (47{35112b74ca1a6bc4decb6697edde3f9edcc1b44915f2ccb9995df8df6b4364bc}) of women with higher incomes (≥ 200{35112b74ca1a6bc4decb6697edde3f9edcc1b44915f2ccb9995df8df6b4364bc} FPL) and those with private insurance (includes employer-sponsored insurance and individually purchased insurance) (47{35112b74ca1a6bc4decb6697edde3f9edcc1b44915f2ccb9995df8df6b4364bc}). The FPL in 2022 for an individual is $13,590 (Figure 2).
Among those who thought they needed mental health care, larger shares of women ages 26-35 (63{35112b74ca1a6bc4decb6697edde3f9edcc1b44915f2ccb9995df8df6b4364bc}) and women ages 36-49 (64{35112b74ca1a6bc4decb6697edde3f9edcc1b44915f2ccb9995df8df6b4364bc}) sought care compared to 55{35112b74ca1a6bc4decb6697edde3f9edcc1b44915f2ccb9995df8df6b4364bc} of women ages 50-64. Larger shares of women enrolled in Medicaid (67{35112b74ca1a6bc4decb6697edde3f9edcc1b44915f2ccb9995df8df6b4364bc}) sought mental health services compared to women who have private insurance (58{35112b74ca1a6bc4decb6697edde3f9edcc1b44915f2ccb9995df8df6b4364bc}) and women who are uninsured (50{35112b74ca1a6bc4decb6697edde3f9edcc1b44915f2ccb9995df8df6b4364bc}) (Figure 3).
A significantly lower share of Asian/Pacific Islander women (40{35112b74ca1a6bc4decb6697edde3f9edcc1b44915f2ccb9995df8df6b4364bc}) say they needed mental health services at some point in the past two years than their White counterparts (50{35112b74ca1a6bc4decb6697edde3f9edcc1b44915f2ccb9995df8df6b4364bc}). Although not statistically significant, smaller shares of Asian/Pacific Islander women report seeking care compared to White women (50{35112b74ca1a6bc4decb6697edde3f9edcc1b44915f2ccb9995df8df6b4364bc} vs. 62{35112b74ca1a6bc4decb6697edde3f9edcc1b44915f2ccb9995df8df6b4364bc}). While the pandemic fueled violence against Asians and subsequently worsened anxiety and mental health for many, studies have shown that Asians reported greater cultural barriers to help-seeking such as family stigma and concerns about “losing face.” Cultural barriers may influence perceived need of care in addition to help-seeking behaviors.
Although the self-reported need for mental health care did not differ between Hispanic and White women (both 50{35112b74ca1a6bc4decb6697edde3f9edcc1b44915f2ccb9995df8df6b4364bc}), smaller shares of Hispanic women (56{35112b74ca1a6bc4decb6697edde3f9edcc1b44915f2ccb9995df8df6b4364bc}) sought care compared to White women (62{35112b74ca1a6bc4decb6697edde3f9edcc1b44915f2ccb9995df8df6b4364bc}). Despite high rates of depression among Hispanic women, studies have shown that stigma and perceived discrimination in health care settings can contribute to underutilization of mental health services within Hispanic communities. Hispanic women also have the highest uninsured rate, which may limit their access to care.
Among the 50{35112b74ca1a6bc4decb6697edde3f9edcc1b44915f2ccb9995df8df6b4364bc} of women who thought they needed mental health services, half (50{35112b74ca1a6bc4decb6697edde3f9edcc1b44915f2ccb9995df8df6b4364bc}) were able to get an appointment, while another 40{35112b74ca1a6bc4decb6697edde3f9edcc1b44915f2ccb9995df8df6b4364bc} did not try to get mental health services (Figure 4). One in ten (10{35112b74ca1a6bc4decb6697edde3f9edcc1b44915f2ccb9995df8df6b4364bc}) who tried to get care were unable to make an appointment for mental health services. This suggests that the other half of women who report needing care may have unmet mental health needs.
Among all women who thought they needed mental health care and tried to get it in the past two years, nearly half (47{35112b74ca1a6bc4decb6697edde3f9edcc1b44915f2ccb9995df8df6b4364bc}) had to wait less than a month for an appointment (Figure 5). One-quarter (24{35112b74ca1a6bc4decb6697edde3f9edcc1b44915f2ccb9995df8df6b4364bc}) had to wait one to two months, and 13{35112b74ca1a6bc4decb6697edde3f9edcc1b44915f2ccb9995df8df6b4364bc} had to wait more than two months to get care. The remaining 16{35112b74ca1a6bc4decb6697edde3f9edcc1b44915f2ccb9995df8df6b4364bc} of those who sought mental health care could not get an appointment.
Among the 16{35112b74ca1a6bc4decb6697edde3f9edcc1b44915f2ccb9995df8df6b4364bc} of women who needed care, sought care, and were unable to get an appointment for mental health services, the main reasons were limited provider availability and cost barriers. One-third of women who could not get an appointment say the main reasons were that they could not find a provider that was accepting new patients (33{35112b74ca1a6bc4decb6697edde3f9edcc1b44915f2ccb9995df8df6b4364bc}) or that they could not afford the cost of mental health services (33{35112b74ca1a6bc4decb6697edde3f9edcc1b44915f2ccb9995df8df6b4364bc}). Eight percent could not get an appointment in a reasonable amount of time and six percent say they could not find a provider nearby. Another 6{35112b74ca1a6bc4decb6697edde3f9edcc1b44915f2ccb9995df8df6b4364bc} say they could not get an appointment for another reason, such as not wanting to go in-person due to COVID-19.
Our findings on provider availability are consistent with other studies on mental health access. A report from the U.S. Government Accountability Office found that many consumers with health insurance faced challenges finding in-network care. The country also faces a workforce shortage of behavioral health professionals in addition to other challenges with health care infrastructure that exacerbates issues with accessibility.
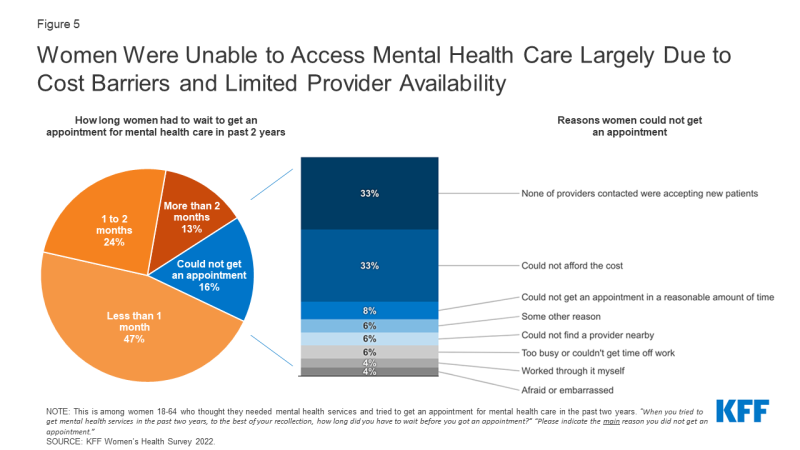
Figure 5: Women Were Unable to Access Mental Health Care Largely Due to Cost Barriers and Limited Provider Availability
Cost and Coverage for Mental Health Services
Among those who sought care but could not get an appointment, one-third (33{35112b74ca1a6bc4decb6697edde3f9edcc1b44915f2ccb9995df8df6b4364bc}) say the main reason was that they could not afford it (Figure 5). Cost remains a barrier to mental health care access for some people with insurance and especially for those who lack coverage. Significantly larger shares of women who are uninsured (60{35112b74ca1a6bc4decb6697edde3f9edcc1b44915f2ccb9995df8df6b4364bc}) say they could not get an appointment due to affordability reasons, compared to those who have health insurance either through private plans (33{35112b74ca1a6bc4decb6697edde3f9edcc1b44915f2ccb9995df8df6b4364bc}) or Medicaid (30{35112b74ca1a6bc4decb6697edde3f9edcc1b44915f2ccb9995df8df6b4364bc}) (Figure 6). There were no significant differences between women who have private insurance and women covered by Medicaid.
These findings on cost barriers are consistent with current literature, which has found that along with provider availability, affordability is one of the most prevalent barriers to mental health care.
While federal laws require special insurance protections such as parity for mental health care, gaps in coverage remain. All state Medicaid programs provide coverage for mental health services, and the Affordable Care Act (ACA) requires most private insurers to cover mental health care. However, the scope of coverage varies, provider networks are limited in many plans, and mental health providers may not accept all insurance plans. Some mental health practitioners do not accept insurance of any kind.
While most privately insured women who received mental health services in the past two years say their provider accepted their insurance for their most recent mental health visit (81{35112b74ca1a6bc4decb6697edde3f9edcc1b44915f2ccb9995df8df6b4364bc}), two in ten (19{35112b74ca1a6bc4decb6697edde3f9edcc1b44915f2ccb9995df8df6b4364bc}) say their provider did not. Among privately insured women who said their provider accepted their insurance, more than half report having out-of-pocket expenses for their most recent mental health visit. More than one-third (36{35112b74ca1a6bc4decb6697edde3f9edcc1b44915f2ccb9995df8df6b4364bc}) say their insurance covered the full cost and 52{35112b74ca1a6bc4decb6697edde3f9edcc1b44915f2ccb9995df8df6b4364bc} say their insurance covered some of the cost. Three percent say their insurance did not cover any of the cost. (Figure 7).
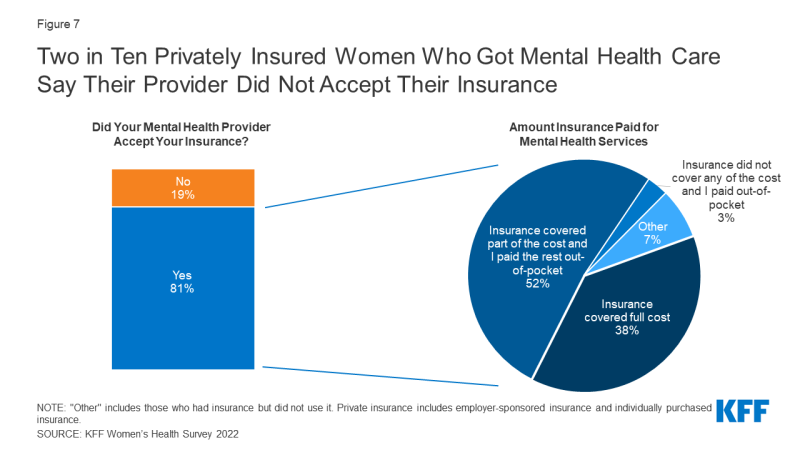
Figure 7: Two in Ten Privately Insured Women Who Got Mental Health Care Say Their Provider Did Not Accept Their Insurance
The Affordable Care Act requires that enrollees in most private health insurance plans have the right to appeal denied claims, though some evidence suggests that many are unfamiliar with appeals processes or are unaware of this protection. Among privately insured women whose insurance was not accepted by their mental health provider, 27{35112b74ca1a6bc4decb6697edde3f9edcc1b44915f2ccb9995df8df6b4364bc} filed a claim with the health insurance plan to try to get reimbursed for some or all the cost (data not shown).
Telehealth
Social distancing during the pandemic contributed to a sharp increase in the provision of telehealth services, widening the access of counseling, therapy, prescribing, and other services via remote methods such as video and telephone. The rapid expansion of telemedicine/telehealth over the course of the COVID-19 pandemic has broadened access to health care for many, including access to mental health services. Mental health services provided via telehealth include speaking to a mental health provider over telephone or video, or through online apps such as Talkspace.
Sixty percent of women ages 18-64 had a telemedicine/telehealth visit in the past two years. Among these women, 17{35112b74ca1a6bc4decb6697edde3f9edcc1b44915f2ccb9995df8df6b4364bc} say the primary purpose of their most recent visit was for mental health services (Figure 8). Accessing mental health care services was the third most common reason for telehealth visits, following annual check-ups (18{35112b74ca1a6bc4decb6697edde3f9edcc1b44915f2ccb9995df8df6b4364bc}) and visits for minor illness or injury (18{35112b74ca1a6bc4decb6697edde3f9edcc1b44915f2ccb9995df8df6b4364bc}). Three in ten women ages 18-25 (29{35112b74ca1a6bc4decb6697edde3f9edcc1b44915f2ccb9995df8df6b4364bc}) say their most recent telehealth visit was for mental health services compared to 20{35112b74ca1a6bc4decb6697edde3f9edcc1b44915f2ccb9995df8df6b4364bc} of women ages 26 to 35, 18{35112b74ca1a6bc4decb6697edde3f9edcc1b44915f2ccb9995df8df6b4364bc} of women ages 36 to 49, and 10{35112b74ca1a6bc4decb6697edde3f9edcc1b44915f2ccb9995df8df6b4364bc} of women ages 50 to 64 and older. A larger share of White women (21{35112b74ca1a6bc4decb6697edde3f9edcc1b44915f2ccb9995df8df6b4364bc}) obtained mental health services at their most recent telehealth visit than Black women (13{35112b74ca1a6bc4decb6697edde3f9edcc1b44915f2ccb9995df8df6b4364bc}), Hispanic women (14{35112b74ca1a6bc4decb6697edde3f9edcc1b44915f2ccb9995df8df6b4364bc}), and Asian/Pacific Islander women (7{35112b74ca1a6bc4decb6697edde3f9edcc1b44915f2ccb9995df8df6b4364bc}).
A larger share of women with Medicaid coverage (22{35112b74ca1a6bc4decb6697edde3f9edcc1b44915f2ccb9995df8df6b4364bc}) report that their most recent telemedicine or telehealth visit was for mental health services than women who are privately insured (15{35112b74ca1a6bc4decb6697edde3f9edcc1b44915f2ccb9995df8df6b4364bc}).
A similar share of women living in rural (23{35112b74ca1a6bc4decb6697edde3f9edcc1b44915f2ccb9995df8df6b4364bc}) and urban/suburban (17{35112b74ca1a6bc4decb6697edde3f9edcc1b44915f2ccb9995df8df6b4364bc}) areas report that the primary purpose of their most recent telehealth or telemedicine visit was for mental health services.
The majority (69{35112b74ca1a6bc4decb6697edde3f9edcc1b44915f2ccb9995df8df6b4364bc}) of women who had a telehealth or telemedicine visit in the past two years for mental health care say the quality of care they received at their most recent visit was the same as an in-person visit for this type of care (Figure 9). One-in-five (19{35112b74ca1a6bc4decb6697edde3f9edcc1b44915f2ccb9995df8df6b4364bc}) report receiving better quality of care during their telehealth visit, while 12{35112b74ca1a6bc4decb6697edde3f9edcc1b44915f2ccb9995df8df6b4364bc} report experiencing worse quality than an in-person visit. These findings suggest the quality of mental health care is typically not diminished when accessing care via telehealth.
Conclusion
The demand for mental health care continues to surge as wait lists for professional help grow. Recent reports reveal that mental health providers across the nation are facing an overwhelming demand for services, leaving many individuals without care. Our survey finds that among the half of women who report that they thought they needed mental health services in the past two years, only half got an appointment for care. Unmet mental health needs are known to affect the overall well-being and productivity of individuals, families, and society, and studies have consistently shown that women are disproportionately affected by these unmet needs. Data from the 2022 KFF WHS underscore that addressing issues with provider availability and cost could improve access to mental health care for some. Our findings suggest that affordability barriers are a substantial obstacle for uninsured women.
In response to the COVID-19 pandemic and other changes in the health policy environment, larger shares of employers began expanding coverage of mental health services by including more providers for in-person and telehealth care. Telehealth and telemedicine services have been recognized as an evolving strategy to increase access to care and address health needs, including care for mental health. We found that most women who received mental health services via telehealth say the quality of care they received was the same as in-person care. Telehealth has and likely will continue to play a role in addressing mental health access concerns for women.
Despite federal and state laws intended to expand and strengthen coverage for mental health care, gaps in coverage and problems with affordability continue to hinder access to mental health services even for those with private insurance and Medicaid. Our survey finds that in addition to challenges obtaining services, many women who have insurance faced at least some out-of-pocket costs for their visit. The findings from the 2022 KFF WHS suggest that future policies affecting telehealth, provider availability, health insurance coverage, and affordability will play a significant role in addressing the demand for mental health care.







